Technology in healthcare has moved from a niche set of tools used in specific departments to a pervasive, patient-centered ecosystem that touches nearly every interaction between clinicians and patients. From virtual visits to AI-powered decision support, the landscape now blends telemedicine, AI diagnostics, and digital health platforms to enhance care delivery. These innovations enable remote patient monitoring, real-time data sharing, and more proactive, personalized care. For sectors across the system, healthcare interoperability is a cornerstone, ensuring data flows securely across EHRs, devices, and apps. Readers will gain insight into how these trends influence outcomes, workflows, and the patient experience.
Beyond the explicit term, the broader landscape can be described as medical technology shaping care delivery, patient engagement, and health data exchange. This shift relies on interoperable systems, clear data governance, and analytics that illuminate patterns across settings, aligning incentives with better outcomes. Digital health ecosystems connect wearables, home monitoring devices, EHRs, and pharmacy data to support seamless care coordination and evidence-based decision making. For patients, these tools translate into actionable insights and safer, more convenient monitoring at home, while clinicians access richer context to inform treatment.
Telemedicine and the new frontier of accessible care
Telemedicine has evolved from a niche capability into a core component of modern care delivery, breaking down geographic barriers and enabling patients to connect with clinicians on their own schedules. This shift is especially meaningful for rural communities and underserved populations, where travel and access to specialists were previously major obstacles. By weaving virtual visits into standard workflows, healthcare teams can triage urgent concerns, support chronic disease management, and deliver timely mental health services with greater consistency.
The broader impact of telemedicine extends beyond convenience. When integrated with electronic health records (EHRs), scheduling systems, and patient portals, virtual care becomes part of a seamless digital health ecosystem. However, its success hinges on reliable connectivity, clear clinical protocols, and robust privacy protections. Effective training for staff and thoughtful patient consent processes are essential to maintain quality and trust in remote interactions.
AI diagnostics: Accelerating insights while safeguarding clinical judgment
AI diagnostics bring advanced pattern recognition to the forefront of clinical decision-making, analyzing imaging, pathology slides, genomics data, and patient records with remarkable speed. In radiology, AI can highlight suspicious regions, helping radiologists prioritize critical cases; in pathology, it can assist with tissue pattern recognition to speed up and standardize interpretations. These capabilities augment clinician expertise, enabling faster triage, more consistent readings, and earlier detection of disease.
The promise of AI diagnostics rests on augmenting human judgment rather than replacing it. Successful adoption requires diverse, high-quality training data, rigorous validation, and ongoing human oversight to manage bias and accountability. Integrating AI tools into workflows with transparent decision support helps clinicians trust and rely on the technology while maintaining a clear locus of responsibility for patient care.
Digital health platforms: Unifying data for patient-centered care
Digital health platforms act as the glue that binds wearables, home monitoring devices, EHRs, pharmacy systems, and laboratory results into a single, accessible interface. For patients, these platforms provide real-time dashboards, medication reminders, and personalized education that empower self-management and engagement. For clinicians, integrated platforms reduce data silos, streamline care coordination, and unlock population health insights that inform proactive interventions.
A strong emphasis on interoperability enables these platforms to deliver on their promise. Standards-based data exchange, such as FHIR, ensures that information moves smoothly between systems, third-party applications, and patient devices. When interoperability is robust, clinicians gain a comprehensive view of a patient’s health, supporting accurate risk assessments, tailored treatment plans, and improved continuity of care across diverse settings.
Remote patient monitoring: Extending care beyond the clinic
Remote patient monitoring (RPM) extends the reach of clinicians by enabling patients to share vital signs, activity data, glucose levels, and other condition-specific metrics from home. These real-time data streams allow clinicians to monitor trajectories, set actionable alerts, and adjust therapies without requiring in-person visits. RPM can be particularly transformative for chronic diseases such as diabetes, hypertension, heart failure, and COPD, helping prevent hospitalizations and enhance quality of life.
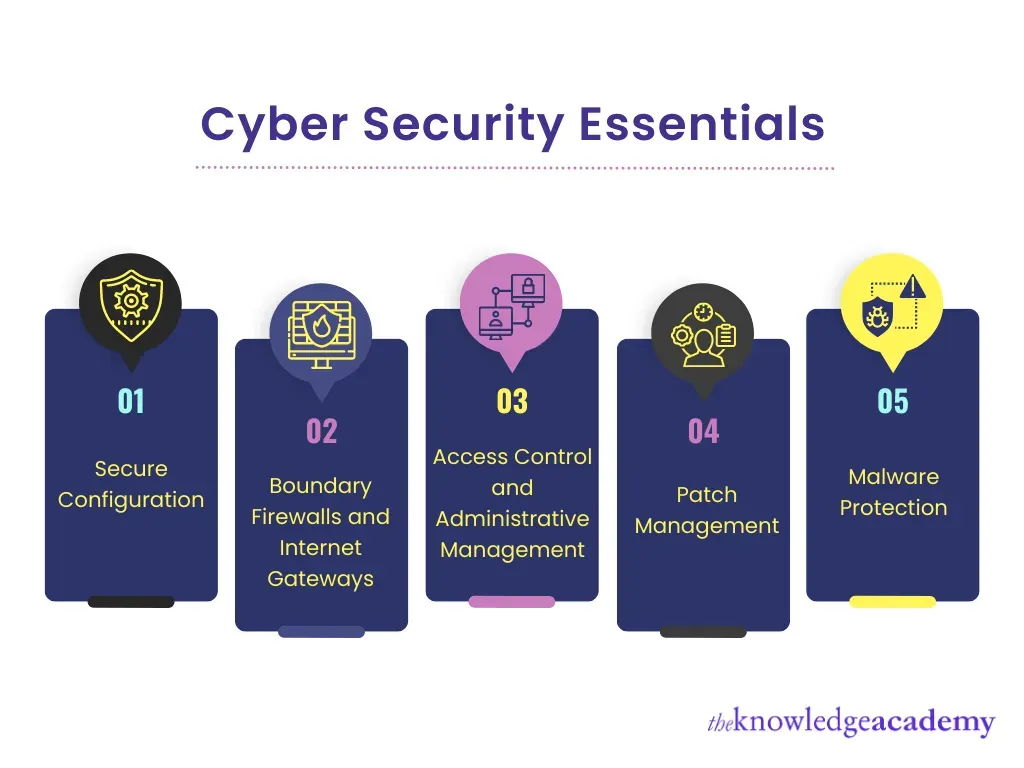
The data produced by RPM also fuels real-world evidence that supports research, regulatory decisions, and personalized care. However, RPM raises considerations around privacy, device security, and informed consent. Organizations must implement robust cybersecurity measures, clear data governance policies, and user-friendly privacy controls to earn and sustain patient trust while ensuring sustainable adoption of RPM programs.
Healthcare interoperability: The backbone of integrated care
Interoperability is the essential enabler of an integrated care ecosystem, allowing clinicians to access a patient’s history, medications, allergies, and care plans from multiple sources. By reducing duplicate testing and preventing adverse events, interoperable systems support safer, more coordinated care across primary, specialty, and post-acute settings. This interconnectedness is a key driver of improved outcomes and more efficient workflows.
Achieving true interoperability requires governance, clear standards, and ongoing collaboration among vendors, providers, and policymakers. Privacy-by-design, robust authentication, and encryption in transit and at rest are critical components of securing patient data as it moves between EHRs, apps, and devices. When systems can share meaningful data securely, clinicians gain a holistic view of patient health, enabling better risk assessment and more consistent care delivery.
Technology in healthcare: Innovation, ethics, and patient trust in a connected system
Technology in healthcare is transforming care delivery, experience, and outcomes across the continuum—from telemedicine and AI diagnostics to digital health platforms and RPM. This transformation enables faster access to care, more precise diagnostics, and proactive management of chronic conditions, ultimately improving patient satisfaction and health metrics. As these tools become more embedded in daily practice, their collective impact on workflows and resource utilization grows ever more significant.
With innovation comes responsibility. Ethical considerations around algorithmic bias, equitable access, and transparent data use require deliberate attention. Privacy-by-design, strong cybersecurity, and patient education about how data are collected and used are essential to maintaining trust. By prioritizing equitable access, secure data practices, and ongoing clinician and patient engagement, the healthcare system can realize the full benefits of technology while safeguarding safety, privacy, and dignity for all patients.
Frequently Asked Questions
How is telemedicine enhancing technology in healthcare to improve access and outcomes?
Telemedicine dramatically expands access in technology in healthcare by enabling virtual visits that cut travel time and wait times. When integrated with EHRs, patient portals, and digital health tools, telemedicine supports better adherence, timely follow-ups, and improved outcomes, especially in rural or underserved areas.
What exactly are AI diagnostics in technology in healthcare, and what benefits and caveats should clinicians consider?
AI diagnostics are AI-driven tools that analyze imaging, pathology, genomics, and patient data to assist clinical decision-making. They can prioritize high‑risk cases and speed up interpretations, but require high-quality data, robust validation, and human oversight to address bias and accountability.
How do digital health platforms support healthcare interoperability in technology in healthcare?
Digital health platforms unify data from wearables, home devices, EHRs, labs, and pharmacy systems into a single interface. Interoperability standards like FHIR enable reliable data exchange, reducing silos and giving clinicians a complete view of a patient’s health to coordinate care.
What role does remote patient monitoring play in technology in healthcare, and what outcomes can it influence?
Remote patient monitoring (RPM) extends care beyond the clinic by using connected devices to track vital signs and condition-specific metrics at home. Real-time data enables timely interventions, can reduce hospitalizations, and supports ongoing management of chronic diseases, while necessitating strong privacy and cybersecurity measures.
What are the key privacy, security, and interoperability considerations when implementing technology in healthcare?
Key considerations include privacy-by-design, strong authentication, encryption in transit and at rest, and transparent data governance. Balancing these security practices with interoperability standards ensures data can flow securely between systems while maintaining patient trust.
How can healthcare organizations balance clinician workload with technology in healthcare, including telemedicine and AI diagnostics?
Balance is achieved by designing workflows that minimize friction, providing just-in-time decision support, and automating routine tasks. Combining telemedicine and AI diagnostics with clinician training and value-based care incentives can improve outcomes while reducing burnout and administrative burden.
| Key Point | Summary | Notes/Examples |
|---|---|---|
| Evolution of technology in healthcare | Technology has moved from niche tools to a pervasive, patient-centered ecosystem touching most clinician–patient interactions, including virtual visits, AI decision support, and digital health platforms. | Covers broad shift toward integrated care, improved outcomes, and enhanced patient experience. |
| Telemedicine: reach and convenience | Virtual visits reduce travel and wait times, expand access to rural/underserved areas, and integrate with EHRs, scheduling, and patient portals. | Used for triage, timely follow-ups, and some mental health services; supports off-hours care. |
| AI diagnostics: accuracy and speed | AI analyzes imaging, pathology, genomics, and patient data to aid early detection and prioritization of high-risk cases. | Augments clinician judgment; risks include bias, data quality, and accountability; requires diverse training data and human oversight. |
| Digital health platforms & interoperability | Platforms unify data from wearables, devices, EHRs, labs, and pharmacies into a single interface for patients and clinicians. | Interoperability via standards like FHIR enables seamless data exchange and comprehensive patient views. |
| Remote patient monitoring (RPM) & real-world data | Connected devices capture vital signs and other metrics at home; real-time views support remote therapies and reduce hospitalizations. | Generates real-world evidence for research and decision-making; raises privacy, device security, and consent considerations. |
| Security, privacy, and patient trust | Privacy-by-design, strong authentication, encryption, and continuous monitoring protect data as digital health expands. | Trust is essential for adoption of telemedicine, AI, and RPM; patient education on data use is important. |
| Clinical workflows & value-based care | Technology should streamline workflows, provide just-in-time decision support, and automate routine tasks to reduce clinician burnout. | Value-based reimbursement incentivizes outcomes improvement and supports robust analytics and training. |
| Ethical considerations & patient-centered design | Address algorithmic bias, access disparities, consent, transparency; design should be inclusive and multilingual/accessible. | Diverse populations in data, user-centered interfaces, and equitable access are key to sustainable adoption. |
Summary
This table highlights how technology in healthcare is expanding from isolated tools to an integrated ecosystem, driving improvements in access, efficiency, and outcomes while presenting challenges around privacy, bias, and usability.