Technology in healthcare has evolved from isolated innovations to a pervasive force that touches almost every patient interaction, clinical decision, and research initiative. From the earliest algorithms assisting radiologists to today’s interconnected networks of digital health tools, technology in healthcare is reshaping how care is delivered, how outcomes are measured, and how healthcare systems operate. The field is now shaped by healthcare technology breakthroughs such as data-driven platforms that unify records, imaging, and analytics, while digital health and health information technology expand access and empower patients and clinicians. Yet adoption introduces questions about privacy, equity, and the practicalities of integrating new tools into busy clinical workflows. Understanding how to balance breakthrough capabilities with responsible use is essential for clinicians, patients, and policymakers alike.
A broader view of this evolution frames it as data-enabled care, where computing power, connectivity, and patient-centered design drive smarter decisions. Terms such as electronic health records, decision-support tools, and interoperable health data ecosystems capture the same core idea without echoing exact keyword phrases. Across care settings, telehealth, remote monitoring, and mobile health apps illustrate how the same movement translates into tangible improvements in access, engagement, and outcomes. Ultimately, success will come from thoughtful implementation, strong governance, and a focus on equity as technology reshapes how clinicians work and patients experience care.
1) Technology in Healthcare: Driving Modern Care and Policy Considerations
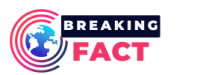
Technology in healthcare now sits at the center of patient care, clinical decision-making, and organizational strategy. It embodies the broader wave of healthcare technology breakthroughs that are reshaping how we diagnose, treat, and monitor health. By integrating digital health tools, wearable sensors, and secure health information technology platforms, modern systems can deliver more timely insights and coordinated care across settings.
However, this progress also requires thoughtful policy and governance to protect privacy, ensure equity, and sustain value. As care becomes more data-driven, stakeholders must balance innovation with clear guidelines on consent, data ownership, and accountability. The result should be an environment where technology in healthcare enhances outcomes while upholding patient trust and access for all.
2) AI Catalysts: How Artificial Intelligence in Healthcare Transforms Diagnostics and Treatment
Artificial intelligence in healthcare is redefining what is possible in diagnostics, triage, and treatment planning. AI-powered pattern recognition in radiology and pathology helps clinicians detect subtle signs that might be invisible to the human eye, enabling earlier interventions and improved outcomes. In oncology and genomics, machine learning supports precision medicine by identifying molecular signatures and tailoring therapies to individuals.
This AI-driven insight is not a substitute for clinician judgment but a powerful augmentation tool. Effective deployment demands rigorous validation, diverse datasets to avoid bias, and thoughtful integration into workflows to prevent cognitive overload. Responsible governance and ongoing monitoring are essential to ensure AI enhances care without compromising safety or equity.
3) Digital Health Expansion: From Patient Portals to Remote Monitoring
Digital health has expanded the reach of care beyond traditional clinics through patient portals, mobile health apps, and telehealth platforms. These tools foster continuous engagement, improve adherence, and empower patients with real-time feedback on their conditions. Wearable sensors and remote monitoring provide actionable data that can guide timely interventions and prevent complications.
As digital health evolves, health information technology infrastructure must support seamless data capture, secure transmission, and meaningful analytics. The goal is to create an ecosystem where patients and clinicians share information effortlessly, enabling proactive care, personalized recommendations, and more efficient care pathways.
4) Telemedicine Benefits and Challenges: Expanding Access While Navigating Barriers
Telemedicine benefits and challenges illustrate both the promise and limits of modern healthcare technology. By breaking down geographic barriers, telemedicine enables timely specialty consultations, reduces travel burdens, and supports remote monitoring for chronic conditions. This expanded access can improve equity by reaching underserved populations who face traditional access challenges.
Yet, successful telemedicine requires reliable connectivity, sustainable reimbursement models, and robust privacy safeguards. Reimbursement policies, licensing considerations, and security requirements must align to sustain long-term telehealth adoption, while clinicians must adapt workflows to maintain efficiency and patient trust.
5) Health Information Technology and Interoperability: Connecting Data for Better Outcomes
Health information technology platforms, including electronic health records and decision support tools, are reshaping how clinicians document care and coordinate services. Interoperability—the ability to share data across systems—remains a critical driver of real-time decision support and population health management. Standards such as FHIR and HL7 underpin this data fluidity, enabling more complete and timely patient records.
While these systems can reduce duplication and errors, they also introduce challenges related to data quality, user experience, and governance. Achieving seamless data exchange requires clear incentives, robust data standards, and ongoing collaboration among vendors, providers, and regulators to ensure that interoperability translates into tangible improvements in outcomes.
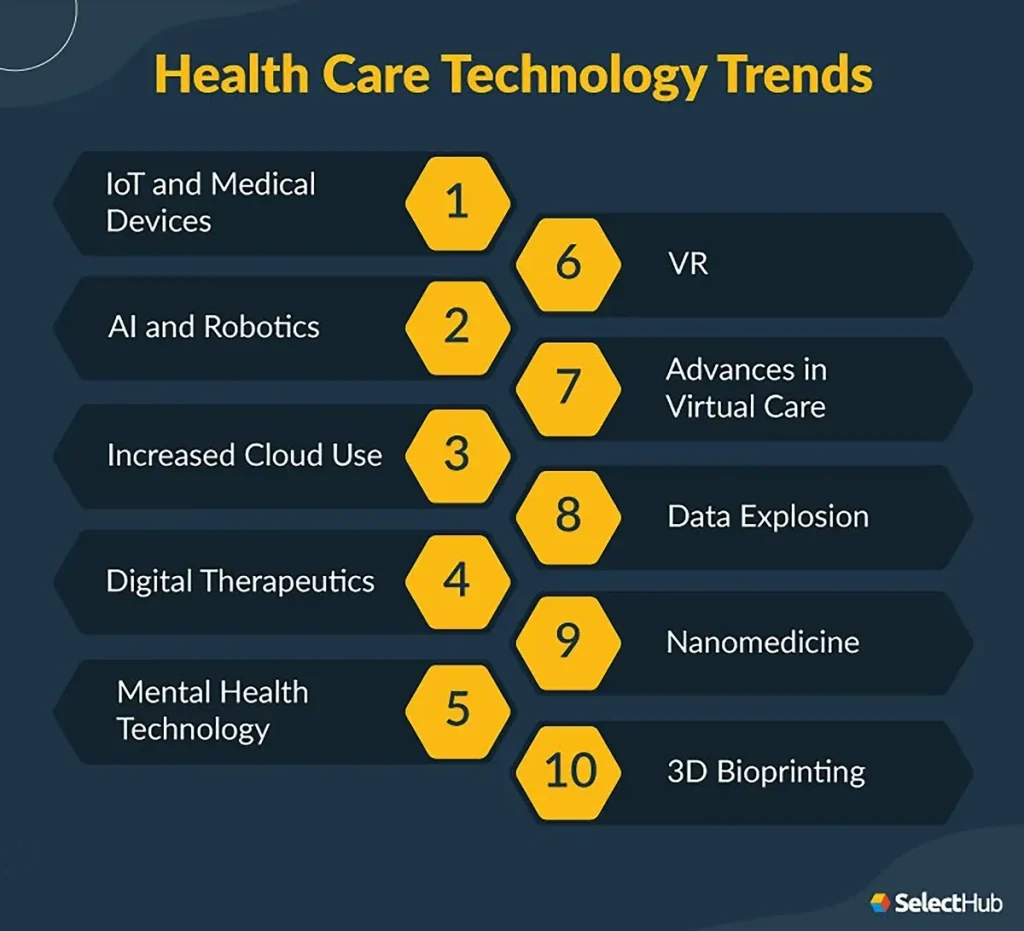
6) Privacy, Security, and Ethics in Healthcare Technology
As patient data moves deeper into digital ecosystems, privacy and cybersecurity become central concerns. Healthcare organizations must deploy robust security architectures, strict access controls, and continuous monitoring to protect sensitive information without hindering clinical work. The stakes are high—breaches can erode trust, disrupt care, and trigger penalties.
Ethical considerations also shape technology adoption. Bias in AI, unequal access to the latest tools, and disparities in digital literacy risk widening health inequities. Addressing these issues requires diverse data, inclusive design, and patient involvement in governance and validation to ensure that breakthroughs translate into equitable, high-quality care for all.
Frequently Asked Questions
How is artificial intelligence in healthcare transforming diagnoses and treatment planning?
Artificial intelligence in healthcare is increasingly used to assist diagnoses, triage, and treatment planning, with AI-driven pattern recognition aiding radiology and pathology for earlier detection. In oncology and genomics, machine learning supports precision medicine by identifying molecular signatures and tailoring therapies to individuals. Realizing these benefits requires high-quality data, rigorous validation, and governance to manage bias, privacy, and safety.
What are the telemedicine benefits and challenges for patients and providers?
Telemedicine benefits include expanded access to specialty care, reduced need for travel, and convenient remote monitoring that supports continuous engagement. Challenges involve ensuring reliable connectivity, creating reimbursement models that recognize telehealth as a core service, and safeguarding patient privacy and data security. Success hinges on thoughtful workflow integration, clinician training, and clear policy guidance.
Why is health information technology essential for modern care delivery?
Health information technology platforms, such as electronic health records, decision support tools, and interoperable data standards, enable more integrated and real-time care decisions. They help coordinate services, reduce duplication, and improve information sharing across teams. Ongoing challenges include user experience, data quality, and achieving seamless interoperability across disparate systems.
How does digital health influence patient engagement and outcomes?
Digital health tools like mobile health apps and patient portals extend care beyond the clinic, enabling continuous engagement and convenient access to information. Wearables and remote monitoring support proactive management of chronic conditions and timely interventions, which can improve adherence and outcomes. Effective digital health strategies depend on user-friendly design and accessible, trustworthy data.
What role do healthcare technology breakthroughs play in precision medicine?
Healthcare technology breakthroughs—such as AI-assisted imaging and genomics-driven analytics—are expanding the possibilities of precision medicine by uncovering molecular signatures and tailoring treatments. These advances empower clinicians with deeper insights but require diverse, representative data, robust validation, and equitable access to translate into real-world improvements.
What governance and implementation practices support responsible health information technology adoption?
Responsible health information technology adoption hinges on strong privacy and cybersecurity protections, clear governance, and ongoing risk management. Adopting and enforcing data standards like FHIR and HL7 improves interoperability, while user-centered design and change management ensure efficient workflows and clinician adoption. Continuous monitoring, training, and governance are essential to sustain safety, quality, and value.
| Aspect | Summary | Notes / Examples |
|---|---|---|
| Evolution of technology in healthcare | From isolated innovations to a pervasive force affecting patient interactions, clinical decisions, and research; ongoing balance between breakthroughs and privacy, equity, and integration. | Privacy, equity, integration considerations |
| Mainstream adoption drivers | Explosion of data, increased computing power, and demand for patient-centered care accelerate adoption. | AI, advanced imaging, wearables, remote monitoring, cloud-based health information systems |
| Key breakthroughs & landscape | AI supports diagnosis and treatment planning; digital health enables access and engagement; wearables and remote monitoring aid chronic care; interoperability underpins real-time decision support. | Radiology/pathology AI; oncology/genomics ML; EHRs, decision support; interoperability standards (FHIR/HL7) |
| Telemedicine benefits & challenges | Breaks geographic barriers and increases access; requires reliable connectivity, appropriate reimbursement, and privacy safeguards. | Timely consults, reduced travel; policy and coverage considerations |
| Practical challenges (privacy, interoperability, cost) | Data privacy, cybersecurity, high-quality data exchange, and cost/workflow integration affect success. | Standards like FHIR/HL7; governance and incentives; potential for clinician burden |
| Implications for patients, clinicians, organizations | Clinicians gain decision support; patients gain engagement; organizations need governance, reimbursement strategies, and culture of learning. | Training, change management, post-market surveillance |
| Future direction | Interoperability, privacy protections, and human-centered design to sustain value; ongoing AI and remote care expansion with responsible deployment. | Bias mitigation, diverse data, co-design with patients |
Summary
Technology in healthcare is a powerful driver of progress, enabling more precise diagnoses, personalized treatments, and easier access to care. The field combines notable breakthroughs—from AI and digital health platforms to telemedicine and health information systems—with challenges around privacy, interoperability, cost, and ethics. By aligning innovation with strong governance, user-centered design, and equitable access, the healthcare system can harness the full potential of technology in healthcare to improve patient outcomes and transform the care experience for generations to come.