Health screenings are a cornerstone of preventive care, helping you catch potential issues before they become serious. By focusing on preventive care tests and timely checks, you gain clarity about what needs attention and when. A clear screening schedule empowers you to coordinate with your clinician and stay on track across adulthood. Knowing your age-specific screenings and the associated risk factors supports early detection and smarter health decisions. This guide outlines how to approach screening, choose appropriate tests, and build a practical plan you can follow with confidence.
Viewed through different lenses, this topic centers on preventive checks, routine risk assessments, and wellness evaluations that flag concerns before symptoms appear. Think of it as a tailored monitoring plan where examinations correspond to life stages, with timing guided by guidelines and personal history. Alternative terms such as screening tests, health risk screening, and preventive examinations convey the same core idea while aligning with search intent. By framing conversations around these terms, you and your clinician can map a practical sequence of tests—what to do, when to do it, and why it matters for long-term health. This approach, informed by latent semantic indexing, helps ensure content remains relevant to readers and search engines while preserving clarity and usefulness.
Health screenings: The Foundation of Preventive Care
Health screenings are the cornerstone of preventive care, designed to uncover potential health issues before symptoms appear. Through preventive care tests, you gain a clearer view of your current health status and a path toward early detection, which often means simpler and more effective treatment. Understanding what tests you need and when to have them empowers you to participate actively in decisions with your healthcare provider.
Importantly, health screenings are not diagnostic tools. They flag clues that warrant further evaluation and guide conversations about next steps. When you regularly engage in screening, you reduce the likelihood of surprises and build a proactive approach to long-term wellness, rooted in early detection and thoughtful planning.
Understanding the Screening Schedule: When to Test Across Life Stages
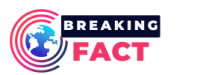
A structured screening schedule ensures you receive the right tests at the right times. The plan should reflect your age, sex, family history, risk factors, and overall health goals, providing a clear roadmap for preventive care tests. Using a schedule helps you coordinate with your clinician so tests like cholesterol checks, blood pressure measurements, diabetes screening, and cancer screenings occur at appropriate intervals.
When you have a defined screening schedule, you’re more likely to stay up to date and avoid gaps in care. It also creates a framework for discussing prevention strategies with your clinician, ensuring tests are spaced appropriately and aligned with your personal health priorities and risk profile.
Age-Specific Screenings: What Tests to Expect by Life Stage
Tests and timing shift as you move through life, making age-specific screenings a practical guide for planning preventive care. In young adulthood, basic checks and risk assessments may apply, while midlife often emphasizes lipid panels, blood pressure, and diabetes risk; discussions about breast or cervical cancer screening may begin depending on guidelines and gender.
In later decades, screenings typically expand to include colorectal cancer screening, bone health considerations, and ocular or dental wellness checks, with ongoing lipid and glucose monitoring. Your clinician will tailor these recommendations to your risk factors and family history, creating a personalized plan that evolves with age and health goals.
Interpreting Screening Results: From Normal Findings to Next Steps
Screening results guide subsequent actions. A normal result usually means you continue with the standard screening schedule, while abnormal or borderline findings often prompt repeat testing, lifestyle adjustments, or referrals for diagnostic testing to confirm a condition.
Understanding what each result means helps you engage in informed conversations with your clinician. Early detection, when feasible, typically translates into broader treatment options and better outcomes, reinforcing the value of staying on track with preventive care tests and follow-up as indicated.
Personalizing Your Screening Plan: Weighing Risk Factors and Shared Decision-Making
Risk factors—such as a family history of heart disease, cancer, or diabetes; tobacco use; obesity; and sedentary lifestyle—shape which screenings you need and how often. Clinicians routinely adjust preventive care tests based on this risk profile, sometimes advising earlier or more frequent screening to improve early detection.
A personalized plan is built through shared decision-making with your healthcare team. Using evidence-based guidelines as a backbone, you can incorporate age-specific screenings, your values, and your life goals to design a practical approach that keeps you engaged and up to date with the right preventive care tests at the right times.
Overcoming Barriers to Preventive Care Tests: Practical Tips for Consistency
Several common barriers—time constraints, cost, fear, and access issues—can derail your screening plans. Practical strategies include scheduling screenings as part of routine care, exploring lower-cost options or community clinics, and enlisting a support person to help with reminders and questions.
Staying proactive requires reminders, clear communication with your clinician, and a willing mindset to address anxiety or confusion about tests. By reducing barriers and reinforcing a steady routine, you enhance your chances of early detection and maintain momentum with your preventive care tests and overall health goals.
Frequently Asked Questions
What are health screenings and why are they important in preventive care tests?
Health screenings are preventive care tests designed to detect diseases or risk factors before symptoms appear. They are not diagnostic tools, but they help flag potential concerns so you and your clinician can intervene early. Regular health screenings support early detection and guide timely actions to protect long-term health.
How can I create a practical screening schedule that fits my age and risk factors?
A practical screening schedule starts with your age, sex, family history, and risk factors. It guides you through the preventive care tests you need at appropriate intervals and helps you stay up to date with health screenings throughout adulthood.
What are age-specific screenings and what tests should I expect at different life stages?
Age-specific screenings vary by life stage. For example, young adults may focus on blood pressure and lifestyle counseling, while midlife often emphasizes lipid and diabetes risk assessments, and older adults may prioritize colorectal cancer screening and bone health checks. Your clinician can tailor age-specific screenings to your personal risk factors.
How do risk factors influence preventive care tests and overall health screenings?
Risk factors such as family history, smoking, obesity, and inactivity can shift recommendations for preventive care tests. If risk factors are present, you may start certain health screenings earlier or screen more frequently; otherwise some tests can be spaced out. Shared decision-making with your clinician helps align tests with evidence-based guidelines.
What should I expect when undergoing health screenings, including preparation and next steps after results?
Preparation for screenings may include fasting, hydration, or avoiding certain meds. At the appointment, you’ll have measurements taken and provide samples as needed. Results determine whether you continue on the standard screening schedule or pursue diagnostic testing, with early detection guiding effective next steps.
What barriers exist to completing preventive care tests and how can I overcome them within a health screenings plan?
Common barriers include time, cost, fear, and access to care. Overcome them by scheduling screenings as part of routine visits, asking about low-cost options, using community clinics, setting reminders, and bringing a support person to appointments.
| Aspect | Key Points | Notes / Why It Matters |
|---|---|---|
| Definition & Purpose | – Health screenings are preventive tests to detect diseases or risk factors before symptoms appear. – They are not diagnostic tools; they help flag potential concerns for early intervention. – Regular screenings can reduce complications and improve outcomes. | Foundation of preventive care; creates a roadmap for long-term health and guided action with your clinician. |
| Scheduling & Routine | – A structured screening schedule should reflect age, sex, family history, risk factors, and health goals. – Regular screening supports early detection and helps you stay on track with tests. | Personalized plans increase adherence and ensure tests are done at the right times; facilitates discussion with your clinician. |
| Age-Life Stages | – Young adulthood (18–39): BP, BMI, lipid panel if risk factors exist; diabetes risk assessment for obesity or family history; cancer prevention counseling. – 40–49: Lipid screening, BP, diabetes screening for at-risk individuals; breast/cervical cancer discussions as appropriate. – 50–64: Colorectal cancer screening may begin around 45–50; continued lipid and glucose testing; bone health, eye and dental wellness. – 65+: Colorectal cancer surveillance as indicated; chronic disease management; cognitive health screening where advised; comprehensive cardiovascular risk assessment. | Guided by guidelines, risk, and history; personalize with your clinician. |
| Risk Factors & Personalization | – Family history of heart disease, cancer, or diabetes; tobacco use; obesity; sedentary lifestyle. – Clinicians adjust tests based on risk; earlier or more frequent testing may be needed; low-risk individuals may space out some tests. | Leads to a tailored plan using evidence-based guidelines. |
| Preparation | – Fasting, hydration, or medication adjustments may be advised pre-test. – Bring a current med list and family history; be ready to provide symptoms. – On test day: measurements, blood/urine samples as needed; cancer screening preps may vary. | Improves test reliability and reduces need for repeats; enables smoother clinical encounters. |
| Interpreting Results | – Normal results: continue standard schedule. – Abnormal/borderline: may require repeats, lifestyle changes, or diagnostic follow-up. – Understanding results supports proactive health decisions and timely care. | Clarifies next steps and reinforces early detection benefits. |
| Barriers & Practical Tips | – Common barriers: time, cost, fear, access. – Tips: schedule with routine care, explore affordable options, bring support, use reminders, discuss anxiety with clinician. | Proactive strategies help maintain adherence and minimize obstacles. |
Summary
Health screenings are a foundational pillar of preventive care. They help identify health issues early, when treatment is often simpler and more effective. Understanding what tests you need and when to have them can empower you to make informed health decisions in collaboration with your healthcare provider.