Technology in healthcare is reshaping the way care is delivered, analyzed, and experienced by patients and providers alike. From telemedicine encounters that bring clinicians into the patient’s home to predictive analytics in healthcare that forecast risks before they become crises, the field is rapidly evolving. This fusion of digital tools, data-driven insights, remote patient monitoring devices, and interoperable data platforms is not merely improving efficiency; it is transforming outcomes, access, and the overall patient experience. In this piece, we explore the benefits and challenges of the healthcare tech shift, and what the future of care might look like for patients and providers alike. The narrative highlights AI in healthcare applications, health data analytics capabilities, and patient-centered strategies that support safer, timelier, and more personalized treatment.
Seen from another angle, this evolution reads as a digital health transformation that relies on connected care, interoperable data, and patient-centered workflows. Terms such as telehealth, e-health, and remote monitoring describe the delivery layer, while data-driven analytics, AI-assisted decision making, and health data analytics describe the insights layer. This framing emphasizes patient engagement, clinician collaboration, and seamless data exchange across platforms. Ultimately, the shift highlights how cloud-based analytics, machine learning, and interoperable standards can create safer, faster, and more accessible care.
Telemedicine and Telehealth: Expanding Access and Convenience
Telemedicine and telehealth are reshaping care delivery by enabling clinicians to reach patients wherever they are. Through synchronous video visits, store-and-forward imaging, and remote consultations, telemedicine reduces travel, shortens wait times, and improves access for rural and underserved populations. The integration with connected devices and mobile apps allows continuous monitoring and timely interventions, turning routine check-ins into proactive care experiences.
As platforms mature and broadband access expands, telemedicine becomes tightly integrated with electronic health records (EHRs) and patient portals, creating a seamless patient journey. This convergence supports not only convenience but also better engagement and treatment adherence, while enabling remote patient monitoring (RPM) data to flow into analytics dashboards that inform proactive care decisions.
Predictive analytics in healthcare: Turning data into proactive care
Predictive analytics in healthcare harnesses statistical models, machine learning, and historical data to forecast future events. Hospitals and clinics use these insights to identify high-risk patients, predict readmission likelihood, and tailor preventive strategies. This capability translates data into action, enabling clinicians to prioritize outreach, allocate resources, and intervene early to prevent deterioration.
Successful analytics depend on clean data, appropriate feature selection, and ongoing validation to avoid biased or inaccurate predictions. In addition to individual patient risk, predictive analytics supports population health management by flagging outbreaks, monitoring adherence trends, and evaluating the impact of quality improvement initiatives, all within a broader health data analytics framework.
Remote patient monitoring: Continuous insights beyond the clinic
Remote patient monitoring (RPM) connects patients with chronic conditions to continuous data streams from wearables, home blood pressure cuffs, glucose trackers, and other devices. RPM helps clinicians observe trends over time, adjust therapies promptly, and intervene before emergencies occur, extending care outside the hospital walls.
For patients, RPM offers reassurance and ongoing support without frequent in-person visits. The data from RPM and telemedicine interactions can feed into centralized analytics platforms, generating timely alerts while reducing unnecessary hospital visits and emergency department utilization. Effective RPM programs rely on reliable data integration, clear patient education, and sensible thresholds to minimize alert fatigue for clinicians.
AI in healthcare and health data analytics: Enhancing clinical decision-making
Artificial intelligence (AI) in healthcare expands clinicians’ capabilities, from imaging analysis that aids radiologists to natural language processing that extracts actionable notes from physician reports. AI-powered decision support can suggest treatment options, flag potential adverse drug interactions, and personalize care pathways based on patient-specific data.
Across the spectrum, health data analytics—encompassing descriptive, diagnostic, predictive, and prescriptive analytics—helps organizations learn from what happened in the past to shape what happens next. Ethical and governance considerations—transparency, fairness, and accountability—are essential to ensure that AI technologies reinforce trust and improve outcomes for all patients.
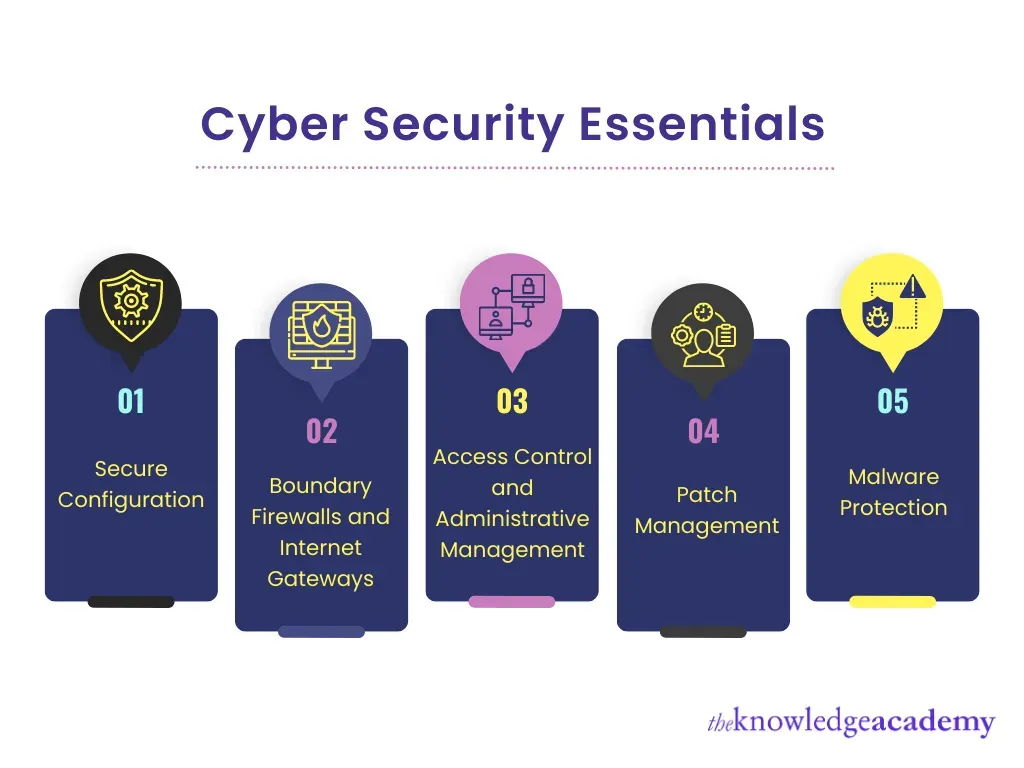
Interoperability, privacy, and security: Making digital health work safely
A core challenge in Technology in healthcare is ensuring that disparate systems communicate effectively. Interoperability enables clinicians to access the right data at the right time, regardless of vendor or platform, with standards such as FHIR (Fast Healthcare Interoperability Resources) supporting data exchange and reducing information silos.
Alongside interoperability, privacy and security measures—encryption, access controls, and robust audit trails—protect patient information in an increasingly connected environment. Balancing ease of access with stringent safeguards is essential to maintain patient trust and comply with regulations.
Technology in healthcare: From telemedicine to analytics and beyond
Technology in healthcare continues its rapid evolution, moving from standalone telemedicine visits toward an integrated ecosystem of devices, data, and AI-powered insights. Telemedicine, remote patient monitoring, predictive analytics in healthcare, and AI in healthcare converge to improve outcomes, accelerate care, and personalize patient experiences, all underpinned by robust health data analytics.
As digital health tools mature, the focus shifts toward equitable access, data quality, privacy, and governance. Sustained impact will depend on thoughtful implementation, clinician training, and patient engagement, ensuring that technology enhances the human elements of care rather than replacing them.
Frequently Asked Questions
In Technology in healthcare, how does telemedicine transform patient access and care delivery?
Telemedicine expands access by connecting patients with clinicians remotely, reducing travel and wait times. In Technology in healthcare, it often integrates with electronic health records and patient portals to create a seamless care journey. While more convenient, success relies on reliable broadband, digital literacy, and robust privacy protections.
What role does predictive analytics in healthcare play within Technology in healthcare?
Predictive analytics in healthcare uses models and historical data to forecast risk, enabling proactive outreach and resource allocation. In Technology in healthcare, these insights help clinicians tailor prevention strategies and prioritize high-risk patients to prevent deterioration. High-quality data and ongoing validation are essential to avoid biased or inaccurate predictions.
How does remote patient monitoring fit into Technology in healthcare, and what benefits does RPM offer?
Remote patient monitoring connects patients with chronic conditions to continuous data streams from wearables and home devices, enabling care outside the clinic. In Technology in healthcare, RPM supports timely adjustments, reduces hospitalizations, and enhances patient reassurance. Effective RPM requires reliable data integration, clear thresholds, and strategies to minimize alert fatigue.
How is AI in healthcare changing decision-making within Technology in healthcare?
AI in healthcare augments clinician decision-making by analyzing complex data, aiding diagnostics, and suggesting treatment options. In Technology in healthcare, health data analytics underpins AI-driven insights, including descriptive, predictive, and prescriptive analyses. Governance, transparency, and fairness are critical to ensure trusted and beneficial use.
Why are interoperability, privacy, and security crucial in the Technology in healthcare landscape?
Interoperability enables timely data sharing across systems using standards like FHIR, accelerating benefits from telemedicine, predictive analytics, and RPM. Privacy and security protections safeguard patient information and regulatory compliance. A balance between easy access and strong safeguards is essential to maintain trust and reduce risk.
What real-world outcomes can be expected from integrating telemedicine, predictive analytics in healthcare, and RPM in Technology in healthcare?
Patients experience shorter wait times, fewer in-person visits, and more proactive care, while clinicians gain deeper insights from data-driven monitoring. Health systems can deploy targeted outreach, reduce complications, and optimize staffing through analytics-informed forecasting. This integrated approach in Technology in healthcare aims to improve outcomes, efficiency, and the overall patient experience.
| Aspect | Key Points | Examples/Notes |
|---|---|---|
| Telemedicine and Telehealth | Expands access and convenience; reduces travel time and wait periods; integrates with EHRs and patient portals | Synchronous video visits; store-and-forward for dermatology or radiology; remote consults with specialists; broader rural access; tighter EHR integration |
| Predictive analytics in healthcare | Forecasts future events; identifies high-risk patients; guides outreach and resource allocation; supports population health | Requires clean data, thoughtful feature selection, and ongoing validation to avoid bias and inaccurate predictions |
| Remote patient monitoring (RPM) | Connects chronic-condition patients to continuous data streams; enables trend observation and timely interventions; reduces hospital visits | Wearables, home BP cuffs, glucose trackers; data integration into EHRs; alert thresholds; minimize alert fatigue with clear protocols |
| AI in healthcare and health data analytics | Enhances diagnostic accuracy and speed; supports decision-making; spans descriptive to prescriptive analytics; raises governance needs | AI in imaging; natural language processing; decision support; emphasis on transparency, fairness, and accountability |
| Interoperability, privacy, and security | Standards-based data exchange; reduces silos; protects patient information | FHIR, encryption, access controls, audit trails; privacy by design; regulatory compliance |
| Real-world impact | Improved outcomes, efficiency, and patient experience; proactive interventions; data-driven staffing | Shorter wait times; fewer hospital visits; better adherence and patient engagement |
| Challenges and considerations | Equity, bias, human factors; ongoing privacy and cybersecurity concerns; workload and change management | Address disparities in access; ensure data quality; provide training and support for clinicians and patients |
| Case examples and practical applications | Illustrative scenarios where telemedicine pairs with analytics and RPM to extend care | Rural telehealth programs with predictive outreach; AI-assisted imaging; integrated RPM workflows |
| Future outlook | Continued AI advancement; wider data exchange; broader digital health services | Deeper primary-care integration; expanded RPM; governance and equity considerations |
Summary
Technology in healthcare is transforming the way care is delivered and experienced. It integrates telemedicine, RPM, predictive analytics, and AI-driven insights to enable proactive, personalized, and accessible care across settings. While challenges remain—privacy, interoperability, equity, and governance—the potential benefits in outcomes, efficiency, and patient experience are compelling. Thoughtful, collaborative implementation will be essential to ensure that Technology in healthcare remains trustworthy, ethical, and centered on patients as care continues to evolve.