Technology in Healthcare is reshaping how care is delivered, diagnosed, and managed today, placing patients at the center of every decision. From digital health platforms that collect and interpret data to telemedicine that extends care beyond hospital walls, these tools redefine access and coordination. When Technology in Healthcare is paired with AI in medicine and robust clinical decision support, clinicians gain faster, more accurate insights, and healthcare interoperability across settings improves. These capabilities elevate patient outcomes, reduce waste, and create more reliable workflows across primary, acute, and post-acute care. To maximize benefit, organizations should implement these tools with thoughtful governance, privacy protections, and continuous measurement of impact.
Viewed through the lens of modern health technology, the care landscape is defined by integrated data, remote interactions, and patient empowerment. Digital innovations in care delivery—ranging from wearable sensors to cloud-based analytics—support evidence-based decisions and faster treatment pathways. Clinical decision support, AI-powered analysis, and interoperable data exchanges help teams coordinate across disciplines and settings. For patients, telemedicine visits, real-time monitoring, and accessible health information foster engagement and convenience. As adoption evolves, governance, security, and equity considerations will shape how these advances translate into sustainable improvements.
Technology in Healthcare: From Digital Health to AI-Driven Outcomes
Technology in healthcare encompasses the full spectrum of devices, software, networks, and data ecosystems that support modern care delivery. Digital health platforms collect, aggregate, and interpret patient information to guide decisions, while telemedicine extends access beyond traditional settings. Artificial intelligence (AI) in medicine, including clinical decision support, helps clinicians interpret complex data, recognize patterns, and tailor interventions to individual patients.
This technology-driven landscape is not about replacing clinicians; it is about augmenting expertise with data-driven insights, automation, and seamless information exchange. When deployed thoughtfully, it strengthens diagnostic accuracy, accelerates treatment, and improves care coordination across multiple settings, from primary care to specialty services. The overarching goal remains to enhance patient outcomes while maintaining safety, privacy, and clinician engagement.
Furthermore, interoperability and secure data exchange underpin these advances. Standardized data formats, open interfaces, and interoperable systems enable a continuous, patient-centered journey where information flows securely between providers, laboratories, pharmacies, and patients themselves. This foundation supports scalable improvements in quality, efficiency, and equity in care.
Digital Health and Data Analytics: Turning Data into Action
Digital health and data analytics transform raw patient information into actionable insights. Real-time monitoring, wearable sensors, and cloud-based data storage generate continuous streams that empower care teams to detect deterioration early, adjust care plans, and prevent adverse events. Predictive analytics help identify high-risk patients who may benefit from proactive interventions, aligning resources with need.
The result is data-driven decision-making that informs protocols, outcomes research, and population health initiatives. When clinicians can leverage robust analytics within clinical decision support tools, they gain confidence in testing, treatment pathways, and escalation plans. This data-centric approach also supports continuous quality improvement and value-based care strategies.
Careful governance, data quality controls, and transparent model evaluation are essential to ensure insights are accurate, unbiased, and applicable to diverse patient populations. Patients benefit from more precise care, while health systems optimize resources and reduce unnecessary variations in practice.
Telemedicine: Expanding Access and Comfort in Care
Telemedicine has emerged as a foundational technology for extending care to rural, underserved, and mobility-challenged populations. By enabling virtual visits for primary care, mental health, chronic disease management, and post-acute follow-ups, telemedicine reduces travel barriers and wait times while maintaining or improving outcomes when integrated with other digital health tools.
Beyond video consultations, telemedicine is enhanced by wearables, patient-reported data, and remote monitoring programs that provide continuous visibility into a patient’s condition. Together, these elements support timely interventions, better adherence to treatment plans, and a more convenient, patient-centered care experience that complements in-person services.
Security, privacy, and workflow integration remain critical as telemedicine scales. Aligning scheduling, documentation, and reimbursement with clinical workflows helps sustain high-quality care and clinician satisfaction in a hybrid care environment.
AI in Medicine and Clinical Decision Support: Enhancing Diagnostics and Treatment
AI in medicine represents a suite of capabilities—from natural language processing that interprets clinical notes to imaging analytics that reveal subtle patterns invisible to the human eye. When integrated with clinical decision support, AI guides clinicians toward the most appropriate tests, therapies, and monitoring strategies, speeding up accurate diagnoses and personalized care.
However, responsible deployment is essential. This includes transparency, ongoing performance validation across diverse patient groups, and clinician oversight to mitigate bias and ensure safety. With proper governance, AI-powered tools can reduce diagnostic errors, optimize treatment pathways, and support clinicians in delivering evidence-based, patient-centered care.
The collaboration between AI, data science, and healthcare teams fosters a continuous learning loop where insights from real-world use refine models and care pathways over time.
Interoperability and Data Exchange: Linking Systems for Seamless Care
Interoperability—the ability of disparate health IT systems to exchange and interpret shared data—is a critical enabler of integrated care. Standardized data formats, open APIs, and collaborative vendor ecosystems ensure that Electronic Health Records (EHRs), laboratory systems, imaging platforms, and patient-facing apps can communicate effectively.
This seamless data exchange reduces redundant testing, minimizes transcription errors, and provides clinicians with timely, comprehensive patient information. Interoperability also fuels population health initiatives, quality improvement, and research by enabling aggregated data to inform evidence-based policy decisions and continuous learning within health systems.
When interoperability is robust, care becomes more coordinated, evidence-based, and efficient, delivering a measurable impact on outcomes and patient experience.
Patient Engagement, Privacy, and Equity in a Digital Health Era
Technology empowers patients to participate more actively in their care through mobile health apps, patient portals, and wearable devices. Real-time access to lab results, medication reminders, and care plans promotes adherence and healthier behaviors. Digital health literacy and user-centric design are essential to ensure these tools are accessible and beneficial for diverse populations.
Privacy, security, and equity are non-negotiables in a digital health ecosystem. Robust data protection, transparent consent practices, and governance measures help sustain patient trust. To avoid widening disparities, organizations must invest in digital access, device availability, and digital literacy initiatives, ensuring that all communities can benefit from technology in healthcare.
Frequently Asked Questions
What is Technology in Healthcare, and why does it matter for patients and clinicians?
Technology in Healthcare refers to the devices, software, networks, and data ecosystems that support care delivery, including digital health tools, AI, and interoperability. It augments clinicians with data‑driven insights, automation, and secure information exchange to improve outcomes and efficiency, rather than replace human judgment.
How do digital health and telemedicine contribute to better patient outcomes in Technology in Healthcare?
Digital health platforms and remote monitoring enable real-time data collection and early detection of health changes, while telemedicine extends care beyond the clinic. Together, they can reduce hospital readmissions and expand access, guided by predictive analytics for proactive care.
How does AI in medicine enhance clinical decision making within Technology in Healthcare?
AI in medicine offers capabilities such as imaging analytics and risk stratification to support faster, more accurate diagnoses. When integrated with clinical decision support and clinician oversight, AI helps tailor tests and therapies while maintaining safety and transparency.
What role does clinical decision support play in technology-enabled care, and how does it impact testing and treatment choices?
Clinical decision support helps clinicians select appropriate tests, personalize treatments, and monitor responses using evidence-based protocols. It improves consistency and speed, but requires ongoing validation, transparency, and clinician oversight to avoid biases.
Why is healthcare interoperability critical for patient care, and how does data exchange improve outcomes?
Healthcare interoperability enables secure data exchange among EHRs, laboratories, imaging systems, and pharmacies, reducing information gaps. This leads to more coordinated care, fewer redundant tests, and stronger population health insights.
What are best practices for implementing Technology in Healthcare responsibly to maximize value and equity?
Best practices include robust privacy and security, governance, staff training, and change management, with a focus on digital health equity and user‑centered design. Measure outcomes regularly to ensure value, safety, and alignment with patient needs.
| Topic | Key Points |
|---|---|
| Introduction | Technology in Healthcare is the backbone of modern practice, enabling digital health platforms, telemedicine, and data-driven care that improve outcomes and efficiency. |
| What is Technology in Healthcare, and Why It Matters? | Engineered devices, software, networks, and data ecosystems support care delivery; includes digital tools, cloud storage, wearables, telemedicine, and AI to augment clinicians with data-driven insights and seamless information exchange. |
| A Pathway to Improved Patient Outcomes | Real-time monitoring and early detection via digital health and data analytics; predictive analytics to identify high-risk patients; AI-driven decision support; interoperable systems for a complete clinical picture. |
| The Efficiency Dividend | Automation of repetitive tasks; streamlined workflows; improved scheduling; AI-assisted documentation; reduced burnout; faster, more consistent care delivery. |
| Telemedicine and Remote Care | Remote care expands access for rural or mobility-impaired patients; supports primary care, mental health, chronic disease management, and follow-ups; often reduces hospitalizations when integrated with wearables and data streams. |
| AI in Medicine and Clinical Decision Support | AI augments clinical reasoning—from NLP in notes to imaging analytics and risk stratification; supports test selection, therapies, and monitoring; requires transparency, bias mitigation, and clinician oversight. |
| Interoperability and Data Exchange | Breaking data silos through standardized formats and open APIs to enable seamless exchange among EHRs, labs, imaging, and patient apps; drives efficiency and learning healthcare systems. |
| Patient Engagement and Experience | Mobile apps, portals, and wearables empower patients with real-time health data and progress; improves adherence; emphasizes digital literacy, accessibility, and equity. |
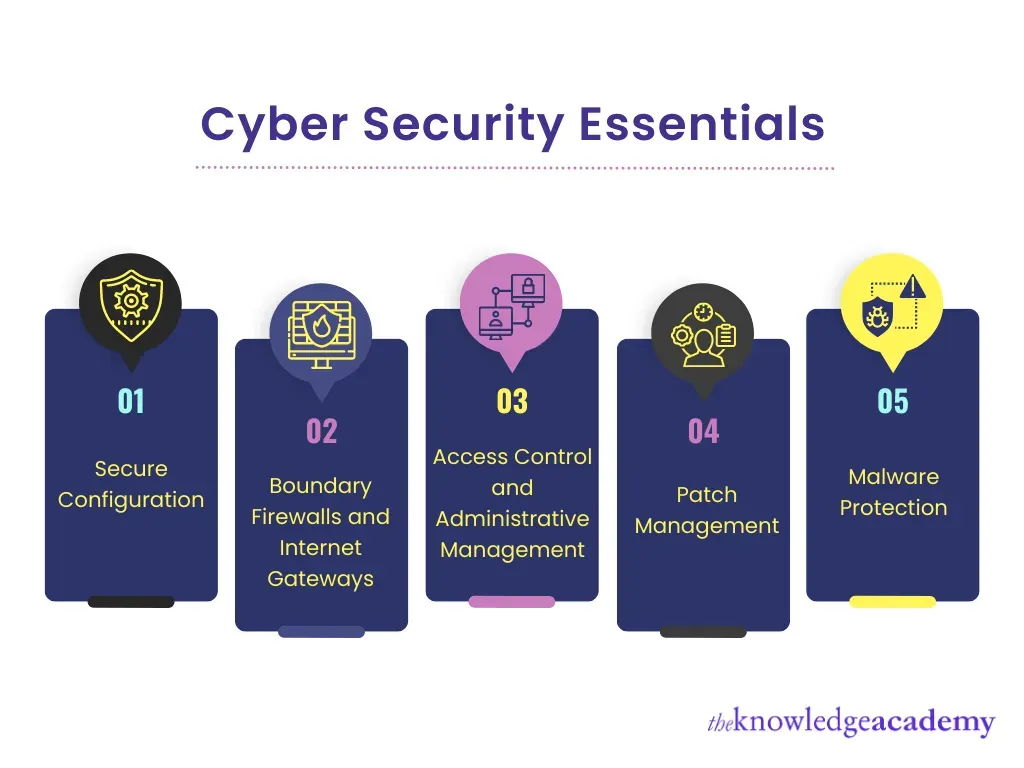
| Challenges and Considerations for Adoption | Costs, training, and change management; cybersecurity, privacy, data governance; potential AI biases; need for clinician oversight and equity-focused implementation. |
| Real-world Examples and Lessons Learned | Interoperable EHRs, decision support, and telemedicine improve diagnostics and guideline adherence; success traits include leadership support, clinician involvement, user-centric design, and outcome measurement. |
| Future Prospects | Wearables, genomics-informed care, real-time analytics, and AI/cloud convergence will enable scalable population health, precision risk stratification, and value-based care. |
Summary
HTML table detailing key points about Technology in Healthcare from the provided base content.